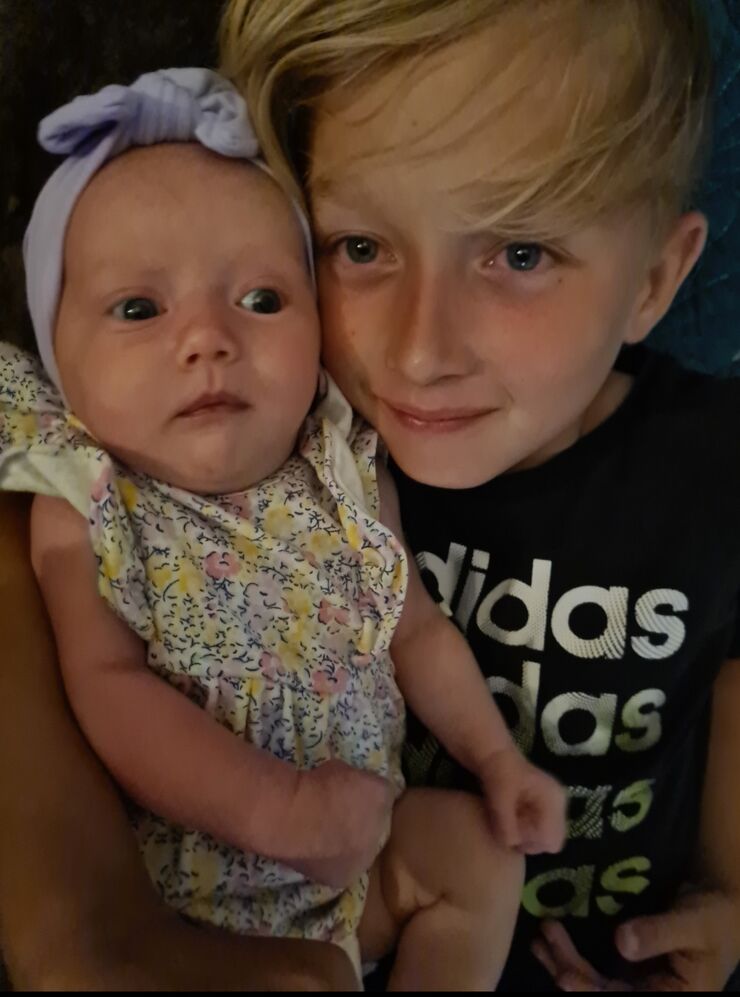
My youngest child was born at 38 weeks and one via c-section, weighing 7lb 5oz. She cried straight away, had suction and seemed okay.
Whilst we were in recovery a doctor came to review her as she was struggling a little with her breathing but all her observations were within normal limits.
I'd been made aware that babies born via c-section before 39 weeks sometimes needed respiratory support but I thought, surely I couldn't be that unlucky.
My partner went home when we were transferred to the ward a few hours after she was born. As soon as we got there the midwives were again concerned about her breathing. She had also been unable to feed properly since she'd been born.
They did a set of observations and her oxygen levels were low as well as her respiratory rate high. This time I had a lot more knowledge as a paediatric nurse and had an idea of what was coming.
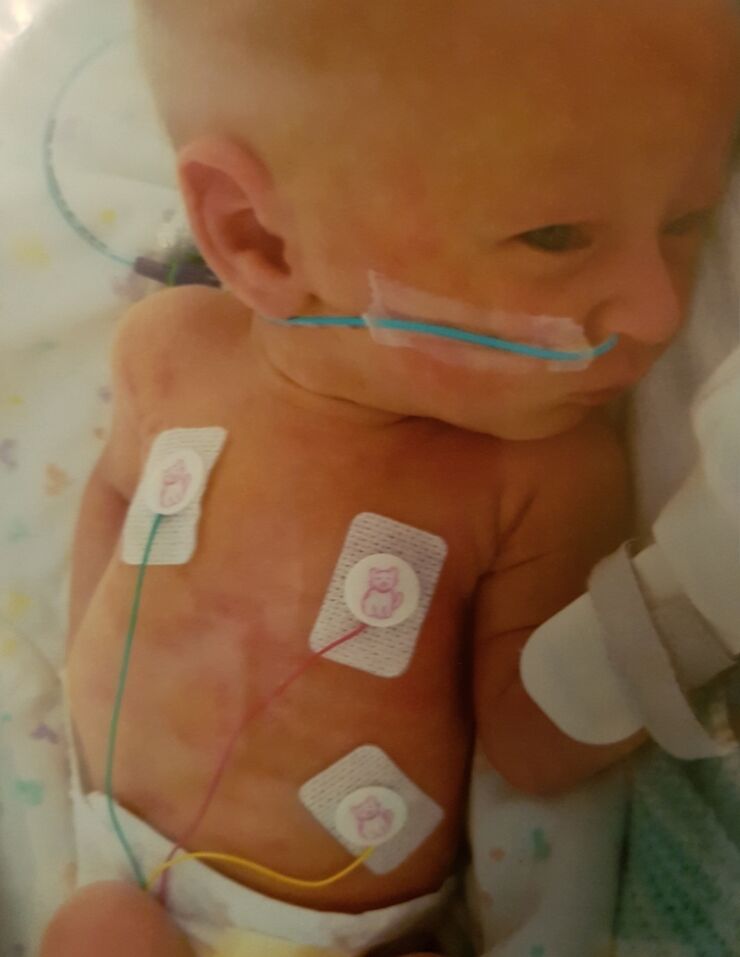
She was taken out of the room for a doctor to review her and the midwives came back a short time later to explain they were taking her to the neonatal unit to be reviewed and that they may insert a cannula and start IV antibiotics.
Although I was worried about her I knew that she was in safe hands. The midwife explained that her oxygen levels had dropped whilst the doctors were trying to cannulate her, so she had been admitted to NICU.
She kindly said that my partner could come back to support me due to what was going on, (visiting was restricted due to Covid-19).
It wasn’t as overwhelming this time when I went to see her. She was on oxygen, as well as IV antibiotics and fluids.
The following morning, she had seemed more alert, looking around and generally seemed more settled than the previous day. I'd gone to the ward to have dinner and when I returned things had changed quite drastically. She was on CPAP her breathing was terrible.
They say knowledge is power but in that situation, knowledge was absolutely terrifying. I even checked her chart to make sure she was definitely my baby and I hadn't gone to the wrong bed space.
Emilia had started to really struggle with her breathing so they'd had to put her on CPAP and she needed a repeat X-ray. They were concerned she may now have a pneumothorax (thankfully she didn't).
I went out of the room to ring my partner and all I could say without crying, was “you need to come to the hospital now”. It was just a case then of waiting to see if she got any worse.
Later that evening a doctor came in and told me that from a surgical point of view I was fit for discharge. I just burst into tears - I couldn't even think about being discharged home with my baby so unwell.