Saturday 16 September started out like any other day. I was 32+4 weeks pregnant and working a shift as a ward sister at my local hospital.
The week before, I had developed bladder infection symptoms and had lost some of my mucus plug. I was monitored on the day assessment unit and was told the baby was happy and healthy. I was reassured that it is normal to lose some mucus as long as it wasn’t blood stained.
During my shift, I took some time out to go and be assessed again because I was feeling really unwell. A doctor and a midwife spent a long time looking me over because urine infections can sometimes lead to premature labour. The baby was once again deemed happy and healthy and I was given antibiotics and told to go home and rest.
I went home for a relaxing bath and what I hoped would be an early night but it all panned out very differently. At around 7.45pm, I suddenly felt a pain in my lower back. I thought this was related to the urine infection but after going to the toilet I lost more of my mucus plug – this time it was blood stained.
I asked my husband to call the midwife for some advice. Before he even had the opportunity to pick up the phone, my waters broke. The pain intensified and I knew that the baby was on his way. My husband called for an ambulance and the operator talked him through how to deliver the baby and what equipment he needed. He had to gather towels and a shoe lace of all things!
My husband successfully delivered our beautiful son Oliver only 11 minutes after my waters broke. We found out later our boy weighed 4lb 11oz – a good weight considering how early he was. Thankfully he also came out screaming which was a huge relief.
The ambulance arrived and took over stabilising Oliver before he was put skin-to-skin and then we were transferred to the local hospital. On arrival, there was a huge team of paediatric specialists and midwives waiting for us. They quickly took our little boy away and set to work on getting him stable enough for the neonatal intensive care unit (NICU). My husband went with them to the unit whilst the midwives checked me over.
It was only when I was left alone that the shock set in. I was a mum. After months of imagining the perfect water birth, this was definitely not what I had planned.

I went to visit Oliver in his incubator two hours later. My heart sunk when I first saw him – a tiny bundle covered in wires and tubes. The nurse let me put my hand into the incubator and touch him. All he had on was a tiny little nappy and was cocooned in a nest of Winnie the Pooh bedding. The nurse said they make the nests to help the babies feel like they are still safely inside the womb.
I didn’t stay on the unit long because there was a wave of activity happening around Oliver. The team said they would come and explain everything about his care once they were finished stabilising him.
Once back on the maternity ward, a midwife taught me how to hand express. I was determined for Oliver to be breast fed although he was tube fed with a special formula until my milk was established enough to be administered via his feeding tube. It felt like the longest, most gruelling task because it can take a while for milk to come in. My husband stayed by my side to support me as I collected tiny amounts of colostrum in a syringe. The amount I was able to produce seemed pointless because it was so minute but I was constantly encouraged by the staff to keep trying. They reminded me how important the “liquid gold” would be for Oliver’s immune system.
I couldn’t sleep that first night because I was so worried and anxious about being separated from Oliver. Unfortunately, the maternity ward was busy so I was put in with the other mums who had their babies at their bedside. I know it couldn’t be helped but it felt like such a kick in the teeth at the time.
At 6.00am, I couldn’t wait any longer and made my way to the NICU with my liquid gold in tow. When I got the unit, the advanced nurse practitioner talked me through everything that they had done to help our little boy. Oliver was now on continuous positive airway pressure (CPAP) to help his immature lungs, phototherapy for his jaundice, and a continuous intravenous drip for hydration. Oliver had also been placed on antibiotics for suspected sepsis.
Being a nurse myself, the word sepsis panicked me. I knew that he was receiving the correct treatment but I couldn’t help but blame my body for putting him here. The nurses reassured me and were so supportive.

I watched on as every hour they pricked his heels to monitor his glucose levels. By lunchtime, Oliver had turned a corner and his blood results were improving. Three days later, I was allowed my first kangaroo care cuddle. I have never been so excited and nervous in all my life. The nurses set me up so I was comfortable and passed me this tiny bundle ensuring that all his tubes and wires were all intact and in position. I sat in silence in my own little precious new born bubble completely mesmerised.
By day four, Oliver was completely off CPAP and my husband finally got to hold him again. I was discharged from the maternity unit the same day and it was horrible leaving without him.
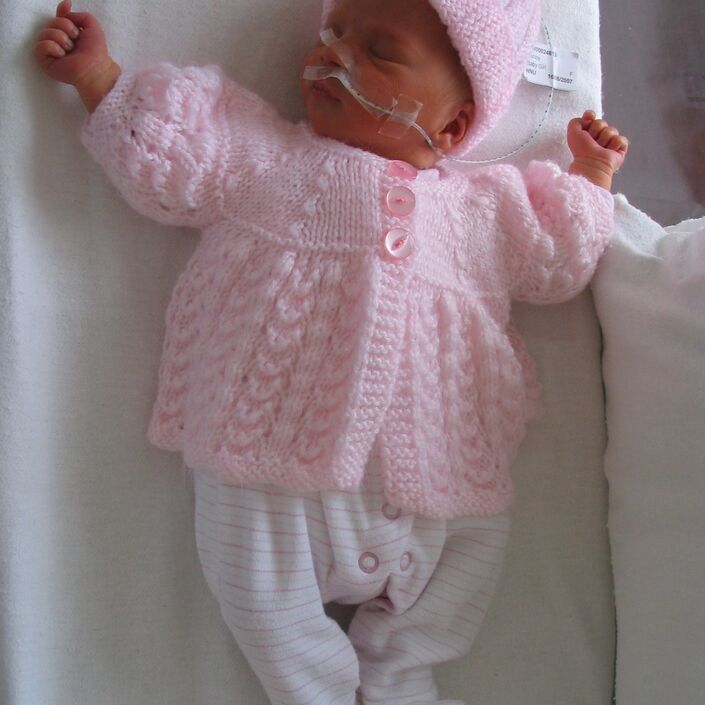
On day six our favourite nurses Bernie and Pru gave me the most amazing news that Oliver would be moved into the nursery into a heated cot and that I could finally dress him. It was so unexpected that I had to pop home and get the freshly washed premature baby grows that we’d bought. It felt so surreal being able to lift Oliver out of the incubator with no tubes or wires, apart from an oxygen monitor attached to his foot, and dress this tiny human.

The nurses were so supportive teaching me how to breast feed my tiny bundle. He could only manage it in short bursts as it was so tiring for him but his latch was perfect. I was shown how to tube feed him and I could carry out all aspects of his care apart from medication. I had all these mothering instincts and feelings come flooding to me and I suddenly felt like I was his mother.
Unfortunately the very next day I came to visit and was told that Oliver’s bilirubin levels had dropped therefore he would need to go back onto phototherapy treatment until back in range. I was so gutted having to strip him back off to his little nappy and place his little eye protection back over his eyes. It was meant to be the day that our parents were going to have their first grandparent cuddles so I had to inform them that they could still visit but wouldn’t be able to hold their new grandson.

At one week old Oliver was back off of phototherapy, the only treatment he was receiving by this point was his tube feeds every three hours which I was doing for him, and once a day caffeine medication, which I learnt is used in premature babies to encourage brain stimulation and to stimulate breathing as premature babies are known to have irregular breathing patterns.
As the days went by, Oliver was getting stronger and stronger. He had managed to establish a good latch and was being breast fed every other feed. I had begun to room in with him on the unit so that we could establish a good feeding routine, ready for discharge home. On day 16 Oliver was able to leave with us.

I am well aware that his stay in hospital was very short compared to many premature and poorly babies, but it doesn't mean that I didn't face the same struggles and the emotional strain. I had put quite a front on during our stay in hospital, and hadn't actually cried at all since his arrival until day 15 when I had the most almighty emotional meltdown. Luckily at the time of our stay the unit was very quiet so the nurses had the time to sit and keep me company. My husband chose to go back to work after four days and take his paternity leave once Oliver could come home, so I spent every day sitting with Oliver for up to 13 hours a day with the odd visitor to pass the hours.
Without the support of all the fantastic nurses, the Bliss support booklets and our amazing friends and family, I think I would have gone into a dark emotional space. I am truly thankful to everyone who helped us get through our time in NICU. To thank everyone at Bliss and our local hospital I arranged a Bliss Little Lights Walk in December. We are lucky that the Royal Sandringham estate is on our doorstep so we completed a lovely walk and raised £480 for Bliss and £250 for our local NICU. Our local NICU has a monthly baby group, where parents can bring their babies to meet, play and to provide continuing support to us. It's so lovely to still see the nurses who helped us, and to also chat to other parents who have been in the exact same position. My husband, Oliver and I will always be eternally grateful for all the care and support we have received.

If you have been affected by any of the issues mentioned in this post and would like support, view our online support pages.