”My little boy Hugo was born at 38+6 weeks of pregnancy via c-section. Initially everything was okay but within an hour a nurse quickly grabbed him from me, saying she was unhappy with his skin colour.
“What I thought was just going to be a quick check-up ended up being the start of every parent’s nightmare.”
Hugo was taken to the special care unit and given oxygen but this did not help and he was soon put on a machine to help with his oxygen levels know as continuous positive airway pressure (CPAP).
“That first night was really difficult and although the midwives put me in a private room, it was hard hearing all the other babies and wishing I had my little boy with me.
“The next day the news wasn't any better. They had done an X-ray which showed Hugo’s lungs weren't inflating properly and his infection indicators had also started to increase.”
Hugo was then transferred to Birmingham Heartlands Hospital for more intensive care.

“Seeing my baby in the neonatal intensive care unit (NICU) was terrifying. It was so noisy - machines beeped constantly and alarms went off. It was dark inside and there were lots of tiny babies.
“The next morning when we got to his incubator his breathing rate was worse and he was still on CPAP. It was at this point I just could not stop crying. The nurse told us he hadn't reacted well to being taken off the CPAP, his infection was getting worse and he wasn't responding to the antibiotics he was on.
“It felt like being hit by a truck. I couldn't understand how this was happening. He was full term - not premature like all the other babies in the room - yet he was really poorly and I couldn't do anything about it. I felt completely redundant as his mum. I couldn't hold him and I wasn't even able to express milk at this point.
“The decision was made to put Hugo on a ventilator - which terrified me - and he had a head scan and lumbar puncture test done to try and determine his infection. Our nurse was lovely and reassured us not to see the ventilator as a step backwards but as a way of giving him a break. He was working so hard to breathe and it was exhausting him.”
The results of Hugo’s lumbar puncture and head scan looked good and the ventilator was stabilising his breathing. Doctors also changed his antibiotics and things began to stabilise. Eventually Hugo’s breathing rate was stable enough that the ventilator could be removed.
“Five days later I got to hold him. When the nurse gave him to me for skin-to-skin it was the best feeling in the world, maybe even better than when he was born. I was still scared of the wires but it was an hour of cuddles I had been waiting for.
“Hugo went from strength to strength. He even pulled out his own feeding tube as if he'd had enough of hospital and wanted to hurry things up. We got the all clear for a discharge 10 days after he was born. Although we were desperate to get him home it was scary knowing that it was just us and no doctors or nurses.
“The NICU - although scary at first - had become our safe place where there was always someone to help and it was scary to step away from that. I'd met so many amazing people - other mums that had been there months, Bliss volunteers that had been through the NICU themselves, nurses working tirelessly, and doctors that really took the time to explain what was happening to our baby. It's a place that will always stick with me, an experience you can't explain to people that haven't seen inside the world of neonatal.”

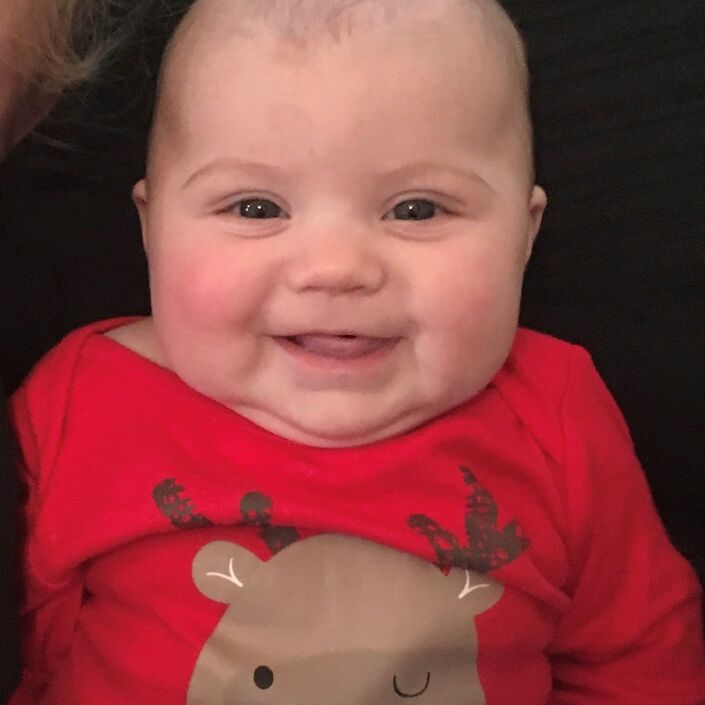
Hugo’s now a healthy and happy seven-month-old, who only needs one more check-up.
Lyn says, “You would never know what a rocky start he had and I can't stop cuddling him.”
If you have been affected by any of the issues mentioned in this post and would like support, view our online support pages.