The pregnancy was the best one I had had: my blood pressure behaved, the baby wriggled lots, morning sickness had subsided by 12 weeks and the scans were all perfect! I was working full time and I planned to start my maternity leave at 36 weeks so I could have longer off after the birth and I knew I would only be restless at home. But my baby had other plans: she arrived a fortnight before I was supposed to go on leave, at just 34 weeks.
I was in work and something just didn’t feel right but I couldn’t put my finger on what it was. I wasn’t in pain, I didn’t feel poorly. The baby had kicked briefly but not as much as usual, and there were still no movements after I had an ice water. I drove to see a midwife and she found a good heartbeat. Phew! But my blood pressure was slightly up and there were some traces of protein in my urine, so we decided I would go to the day unit at our nearest hospital. Hospital number one.
I felt fine while I sat in the corridor outside the ward. But when I was called through to be put on the monitor, I suddenly felt sick, and blacked out. When I came around, I was in a room on the labour ward with my partner on his way.
When our little girl arrived, she wasn’t breathing and was bluey-grey in colour. All I wanted was skin on skin with her and to breastfeed her, but she was whisked away and we didn’t see her for five hours. Later, we were told our baby had been resuscitated and put on a ventilator as she could not breathe on her own. But the hospital did not have the equipment or expertise needed to keep her alive, so we were transferred to Alder Hey Children’s Hospital.
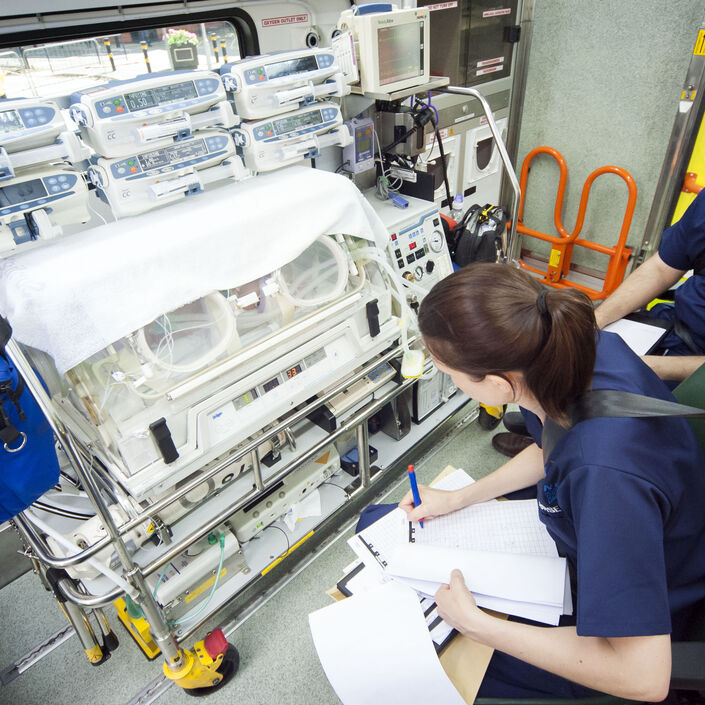
As I got into the ambulance to Alder Hey, with everyone around me looking on sympathetically, my legs felt like jelly. Only one parent could travel in the ambulance so my partner had to find his own way there. I heard the words ‘blue lights – quick as you can!’ I knew the journey was over an hour by car – would we get there quick enough? I was so sore that each bump in the road was agonising; machines were beeping around me; the sirens were so loud. Through a tiny gap in the window, I could see cars pulling over, making way for my baby fighting for her life. But the ambulance team were so calm, and kept chatting to me – I can’t remember what about – to lighten the mood.
I just wanted to have a bath, get in a pair of clean pyjamas, and have a cup of tea and slice of toast on the post-natal ward. But instead, my breasts were leaking, I was still losing blood and I was travelling with total strangers in an ambulance with its blue lights flashing.
At Alder Hey, hospital number two, they soon discovered the problem: our baby had persistent pulmonary hypertension (PPHN), a condition which affects roughly one in five hundred babies, where the pressure in the blood vessels in the lungs doesn’t lower like it should after birth.